The dopamine hypothesis
The dopamine hypothesis is fascinating and the text below is well worth a read.
This hypothesis is based on two main observations:
A bit of history
It is hypothesised that dopamine and dopaminergic mechanisms are central to schizophrenia.
This began with observations that chlorpromazine caused surgical patients to be calm and somnolent, with a relaxed and detached expression. Then, in 1952, Delay showed that within three days, chlorpromazine alleviated hallucinations and stopped internal voices. The extra-pyramidal side effects noted with antipsychotics then led people to make the link with Parkinsons disease and to suggest that dopamine may be involved. In 1963, Carlsson and Lindqvit identified that antipsychotic drugs increased the metabolism of dopamine when administered to animals, thus strengthening the argument. Studies also showed that amphetamine, which increases synaptic monoamine levels, can induce psychotic symptoms.
It was not until the 1970s, however, that the dopamine hypothesis was finally crystallized with the finding that the clinical effectiveness of antipsychotic drugs was directly related to their affinity for dopamine receptors.
At this stage the belief was that the problem related to an excess of dopamine in the brain.
In 1991, Davis introduced the concept of regional specificity. It was clear by this stage that dopamine metabolites were not universally elevated in the cerebrospinal fluid (CSF) or serum of patients with schizophrenia. Also, the focus on D2 receptors was brought into question by findings showing that clozapine had superior efficacy for patients who were refractory to other antipsychotic drugs despite having rather low affinity for and occupancy at D2 receptors.
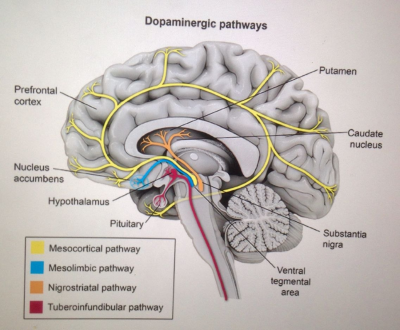
PET studies showed reduced cerebral blood flow in the frontal cortex suggesting regional brain dysfunction in schizophrenia. Hypofrontality in these studies was directly correlated with low CSF dopamine metabolite levels. Because CSF dopamine metabolite levels reflect cortical dopamine metabolism, it was argued that the relationship between hypofrontality and low CSF dopamine metabolite levels indicates low frontal dopamine levels. Thus, there was a move from a one-sided dopamine hypothesis explaining all facets of schizophrenia to a regionally specific prefrontal hypodopaminergia and a subcortical hyperdopaminergia.
It was hypothesized that negative symptoms of schizophrenia resulted from frontal hypodopaminergia, based on the similarities between the behaviour exhibited by animals and humans with frontal lobe lesions and the negative symptoms of schizophrenia. Positive symptoms were hypothesized to result from striatal hyperdopaminergia, based on the findings that higher dopamine metabolite levels are related to greater positive symptoms and response to antipsychotic drug treatment.
Current thinking
It has been shown that acutely psychotic patients show evaluated presynaptic dopamine synthesis (in the striatum). It has also been shown that this correlates with increased levels of dopamine in the synapse.
A modest (10-20%) elevation in striatal D2/3 receptor density in schizophrenia independent of the effects of antipsychotic drugs has been demonstrated (striatal D1 receptor densities are unaltered) and this elevation may be regionally specific because these increases are not seen in the extrastriatal regions.
Various studies show that at clinical doses, all currently licensed antipsychotic drugs block striatal D2 receptors.
A number of environmental factors, such as pregnancy/obstetric complications, stress, migration, and childhood abuse have been shown to lead to dopaminergic overactivity.
A number of psychoactive substances also increase the risk of schizophrenia. Cannabinoid agonists have been shown in animals to increase striatal dopamine release. PET imaging work has shown that even a few doses of a stimulant may sensitize the striatal dopamine system and can lead to enduring increases in dopamine release to amphetamine even after many months of abstinence.
In summary, psychosis appears to result from excessive dopamine activity in the striatum. The negative symptoms seen in schizophrenia appear to result from too little dopamine activity in the frontal lobe. Antipsychotic medications appear to help by countering the effects of increased dopamine by blocking post-synaptic D2 receptors in the striatum.
Above adapted from Oliver D (2009) The Dopamine Hypothesis of Schizophrenia: Version III The Final Common Pathway. Schizophr Bull (2009) 35 (3): 549-562
Note: The striatum, is a subcortical part of the forebrain. It receives input from the cerebral cortex and is the primary input to the basal ganglia system. The striatum is divided by a white matter tract called the internal capsule into two sectors called the caudate nucleus and the putamen.
This hypothesis is based on two main observations:
- it is possible to induce a psychotic episode in healthy subjects with pharmacological dopamine agonist
- all effective antipsychotic drugs provide at least some degree of D2-type dopamine receptor blockade.
A bit of history
It is hypothesised that dopamine and dopaminergic mechanisms are central to schizophrenia.
This began with observations that chlorpromazine caused surgical patients to be calm and somnolent, with a relaxed and detached expression. Then, in 1952, Delay showed that within three days, chlorpromazine alleviated hallucinations and stopped internal voices. The extra-pyramidal side effects noted with antipsychotics then led people to make the link with Parkinsons disease and to suggest that dopamine may be involved. In 1963, Carlsson and Lindqvit identified that antipsychotic drugs increased the metabolism of dopamine when administered to animals, thus strengthening the argument. Studies also showed that amphetamine, which increases synaptic monoamine levels, can induce psychotic symptoms.
It was not until the 1970s, however, that the dopamine hypothesis was finally crystallized with the finding that the clinical effectiveness of antipsychotic drugs was directly related to their affinity for dopamine receptors.
At this stage the belief was that the problem related to an excess of dopamine in the brain.
In 1991, Davis introduced the concept of regional specificity. It was clear by this stage that dopamine metabolites were not universally elevated in the cerebrospinal fluid (CSF) or serum of patients with schizophrenia. Also, the focus on D2 receptors was brought into question by findings showing that clozapine had superior efficacy for patients who were refractory to other antipsychotic drugs despite having rather low affinity for and occupancy at D2 receptors.
PET studies showed reduced cerebral blood flow in the frontal cortex suggesting regional brain dysfunction in schizophrenia. Hypofrontality in these studies was directly correlated with low CSF dopamine metabolite levels. Because CSF dopamine metabolite levels reflect cortical dopamine metabolism, it was argued that the relationship between hypofrontality and low CSF dopamine metabolite levels indicates low frontal dopamine levels. Thus, there was a move from a one-sided dopamine hypothesis explaining all facets of schizophrenia to a regionally specific prefrontal hypodopaminergia and a subcortical hyperdopaminergia.
It was hypothesized that negative symptoms of schizophrenia resulted from frontal hypodopaminergia, based on the similarities between the behaviour exhibited by animals and humans with frontal lobe lesions and the negative symptoms of schizophrenia. Positive symptoms were hypothesized to result from striatal hyperdopaminergia, based on the findings that higher dopamine metabolite levels are related to greater positive symptoms and response to antipsychotic drug treatment.
Current thinking
It has been shown that acutely psychotic patients show evaluated presynaptic dopamine synthesis (in the striatum). It has also been shown that this correlates with increased levels of dopamine in the synapse.
A modest (10-20%) elevation in striatal D2/3 receptor density in schizophrenia independent of the effects of antipsychotic drugs has been demonstrated (striatal D1 receptor densities are unaltered) and this elevation may be regionally specific because these increases are not seen in the extrastriatal regions.
Various studies show that at clinical doses, all currently licensed antipsychotic drugs block striatal D2 receptors.
A number of environmental factors, such as pregnancy/obstetric complications, stress, migration, and childhood abuse have been shown to lead to dopaminergic overactivity.
A number of psychoactive substances also increase the risk of schizophrenia. Cannabinoid agonists have been shown in animals to increase striatal dopamine release. PET imaging work has shown that even a few doses of a stimulant may sensitize the striatal dopamine system and can lead to enduring increases in dopamine release to amphetamine even after many months of abstinence.
In summary, psychosis appears to result from excessive dopamine activity in the striatum. The negative symptoms seen in schizophrenia appear to result from too little dopamine activity in the frontal lobe. Antipsychotic medications appear to help by countering the effects of increased dopamine by blocking post-synaptic D2 receptors in the striatum.
Above adapted from Oliver D (2009) The Dopamine Hypothesis of Schizophrenia: Version III The Final Common Pathway. Schizophr Bull (2009) 35 (3): 549-562
Note: The striatum, is a subcortical part of the forebrain. It receives input from the cerebral cortex and is the primary input to the basal ganglia system. The striatum is divided by a white matter tract called the internal capsule into two sectors called the caudate nucleus and the putamen.
 |
